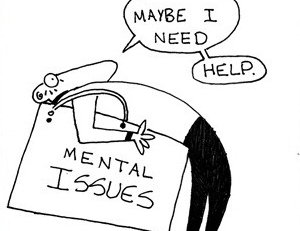
Within the demanding world of healthcare, where medical professionals and therapists dedicate their lives to the well-being of others, a silent struggle often goes unnoticed- the battle of their own mental health. Therapists are often perceived as bastions of strength and stability, yet behind closed doors, many wrestle with their own emotional burdens. The nature of their profession exposes them to client’s trauma and suffering, which can take a toll on their mental and emotional resilience. Additionally, the pressure to maintain the facade of competence and composure can exacerbate feelings of isolation and burnout.
There have been surveys that found high rates of burnout among medical practitioners, including psychiatrists and mental health professionals (Yasgur, 2019; Ramberg and Wasserman, 2000). There is a high suicide rate amongst mental health professionals, where Yasgur from her study indicate 30 percent have felt suicidal and 4 percent have made a suicide attempt (Yasgur, 2019).
Therapists are naturally compassionate, which is often what draws them to this profession. However, the sense of exhaustion mental health professionals feel caused by overexposure to distress is referred to as ‘therapists’ burnout’ or ‘compassion fatigue’. Therapists’ burnout manifests as feelings of cynicism, detachment, and reduced sense of accomplishment. Conversely compassionate fatigue also known as ‘secondary traumatic stress’ occurs when therapists experience emotional and psychological distress due to empathizing with their client’s suffering. This can further lead to depletion of emotional reserves, resulting in symptoms such as emotional numbness, irritability, and a diminished ability to empathize.
Despite the prevalence of mental health challenges among medical professionals and therapists, there exists a pervasive stigma surrounding mental illness within the healthcare community. Seeking help for mental health concerns is often viewed as a sign of weakness or incompetence, leading many individuals to suffer in silence rather than seek the support they need. This stigma not only perpetuates the myth of invincibility among medical professionals and therapists but also creates barriers to accessing mental health resources and support services. Fear of judgement, professional repercussions and concerns about confidentiality further deter individuals from seeking help, exacerbating their mental health struggles. Furthermore, societal stigma surrounding mental illness and therapy perpetuates misconceptions about the field, leading to lack of recognition and appreciation for the vital work that mental health professionals do.
When therapists encounter violence from patients, it profoundly affects their sense of safety and well-being leading to problems like anxiety. They may further trigger feelings of immense fear, helplessness, and even Post Traumatic Stress Disorder symptoms in therapists. Moreover, facing criticism despite their best efforts, constantly striving to help clients only to face negative feedback or blame is emotionally draining and demoralizing. Additionally witnessing long term patients experience relapse especially in an inpatient facility where intensive work is being done with the patients and families can lead therapists to question the effectiveness of their interventions and experience feelings of disappointment or hopelessness.
Yet, amidst the shadows of this struggle, glimmers of hope emerge. There have been efforts made to shed light on the mental health challenges faced by medical professionals and therapists, breaking down the barriers of silence and shame. There have been initiatives by peer support groups, mental health awareness campaigns and workplace wellness programs providing much needed resources and avenues for support.
While progress has been made there are still areas that require attention and improvement. One crucial aspect is the destigmatisation of mental health issues within the healthcare community itself. Additionally, there is a need for ongoing education and training on mental health, self-care and resilience building strategies. There needs to be comprehensive training programs that equip healthcare professionals with practical tools to manage stress, prevent burnout and prioritizing their own mental well being like mindfulness, self-compassion, setting boundaries, regular exercises, healthy lifestyle choices, seeking support and reflective practices to enhance self-awareness.
Furthermore, creating a culture of openness and fostering environment where professionals feel comfortable discussing mental health concerns without fear of judgement and repercussions. There have been systematic issues such as inadequate staffing, high patient caseloads and limited resources that are crucial to mitigating the factors contributing to mental health challenges among medical professionals. Allocating sufficient resources to mental health services and implementing measures to reduce workload can help alleviate the burden on healthcare professionals and promote better mental well-being.
In conclusion, it’s crucial to acknowledge the often-thankless nature of mental health treatment, where the results are not always as visible or immediate as those of physical ailments like diabetes, cholesterol, thyroid and among others. Mental health requires patience, understanding and consistent support yet it is often unappreciated in comparison. Compounded by the pervasive stigma surrounding mental illness, people tend to seek help only when the situation is dire, placing additional strain on both patients and medical professionals. In the context of Nepal, where cultural attributes towards mental health may further compound these challenges. It’s important to recognize and address the unique obstacles faced by mental health professionals as they work tirelessly to provide essential care and support.
The author is the Chief Executive Officer of Chaitanya Institute for Mental Health, Nepal. Contact: chaitanyarehabnepal@gmail.com
- How To Practice Emotional First Aid?
- May 13, 2023
- Mind Your Plate
- Jun 07, 2021
- The Simple Act Of Kindness Could Promote Both Mental And Physical Health.
- Oct 10, 2020